In 2023, synthetic opioids (primarily fentanyl) caused approximately 74,702 deaths, accounting for nearly 70% of all overdose fatalities in the United States. Understanding fentanyl’s addictive power isn’t just academic anymore, it’s critical for saving lives as this drug tears through communities nationwide.
What makes fentanyl so dangerously addictive is how it hijacks both the brain’s reward system and withdrawal pathways simultaneously. Research from the National Institute on Drug Abuse shows fentanyl activates mu-opioid receptors in two distinct brain regions. The ventral tegmental area creates intense euphoria. The central amygdala drives severe withdrawal symptoms. This double hit creates a powerful drive to chase the high and an equally intense need to avoid withdrawal.
The widespread presence of fentanyl in counterfeit pills and street drugs has led to unintentional exposure among people who believed they were using less potent substances. Many people become dependent without knowing they’ve even taken fentanyl, dealers routinely mix it into cocaine, heroin, or counterfeit pills. At Peak Path Health, we address this crisis through comprehensive fentanyl addiction treatment that targets the drug’s unique impact on brain chemistry.
How Severe is the Fentanyl Crisis in America?
The fentanyl epidemic has hit record levels across the United States. Data from the Centers for Disease Control (CDC) shows roughly 107,543 total drug overdose deaths in 2023. About 81,083 involved opioids. California leads the nation with 12,835 overdose deaths between May 2023 and May 2024.
The crisis has hit young people especially hard. Among youth ages 10 to 19, fentanyl-related deaths in California jumped from 36 in 2018 to 261 in 2020 (a 625% increase). These numbers show how fast fentanyl has taken over the illicit drug market, highlighting the urgency of the situation.
How Did Fentanyl Get to be a Problem?
Doctors originally developed fentanyl to manage severe pain in cancer patients and people recovering from major surgeries. The shift to illicit use began when illegal labs started churning out fentanyl and cutting it into street drugs to boost potency cheaply.
Illicit fentanyl production has exploded. The California National Guard seized over 62,000 pounds of fentanyl in 2023, representing more than a 1,000% increase compared to 2021 seizures. Counterfeit pills designed to mimic real prescriptions now routinely contain lethal doses of fentanyl. Users have no idea what they’re taking.
What Is Fentanyl?
Fentanyl is a lab-made opioid designed to manage severe pain. Unlike morphine or heroin, it’s fully synthetic, not derived from poppy plants. Doctors prescribe fentanyl in patches, lozenges, and injectable forms for patients recovering from major surgeries or experiencing advanced cancer pain.
On the street, fentanyl shows up as powder, pills, or liquid, often mixed into other drugs. Here’s why fentanyl is so deadly:
- Morphine: Fentanyl is 50 to 100 times more potent
- Heroin: Fentanyl is approximately 50 times stronger
- Fatal dose: As little as 2 milligrams, equivalent to a few grains of salt, can cause death
What are the Causes and Risk Factors for Fentanyl Abuse?
Fentanyl addiction doesn’t happen in a vacuum, it stems from biological, psychological, and environmental factors working together. Certain factors raise a person’s risk:
- Prior opioid use: If a person has taken prescription painkillers before, their brain has already adapted to opioids, making fentanyl dependence more likely.
- Genetic factors: A family history of addiction can make you more vulnerable through inherited traits that affect how your brain processes rewards
- Mental health conditions: Depression, PTSD, and anxiety often accompany fentanyl use, and when left untreated, they increase relapse risk.
- Environmental factors: Poverty, unstable housing, and social circles where drug use happens all raise your exposure risk significantly
Chronic pain is another major risk factor. People prescribed opioids for pain sometimes end up misusing fentanyl. Trauma and childhood adversity often lead people to self-medicate with drugs like fentanyl.
What Does Fentanyl Do to the Brain and Body?
Fentanyl latches onto mu-opioid receptors, the brain’s pain and emotion control centers. When fentanyl hits receptors in the ventral tegmental area, it triggers a cascade. GABA neurons release, flooding the nucleus accumbens with dopamine, the brain’s pleasure chemical. This dopamine flood creates fentanyl’s intense high.
Fentanyl rewires the brain fast. Each use reshapes neural pathways, making the urge to seek and use fentanyl stronger. These brain changes stick around even after you quit. That’s why relapse rates stay high in early recovery.
Immediate effects include:
- Intense euphoria and feelings of well-being
- Complete blocking of pain signals
- Slowed breathing that can become life-threatening
Brain changes involve:
- Decreased natural dopamine production
- Tolerance development requires larger doses
- Withdrawal activation triggers fear and anxiety responses
What are the Long-Term Effects of Fentanyl?
Long-term fentanyl use damages multiple body systems permanently. The brain changes fueling addiction reach far beyond that first high.
| Physical Effects | Mental and Social Effects
|
| Respiratory damage and weakened breathing | Depression and persistent mood disorders |
| Organ damage from repeated low oxygen | Memory problems and impaired decision-making |
| Cardiovascular problems and heart disease risk | Relationship breakdown and social isolation |
| Immune system suppression | Financial instability and legal consequences |
These effects trap people deeper in addiction by giving them more reasons to keep using. Depression from scrambled brain chemistry pushes users toward more fentanyl. Broken relationships pile on more emotional pain.
Why is Fentanyl so Addictive and Dangerous?
Fentanyl hits mu-opioid receptors in two brain regions at once, triggering intense euphoria and brutal withdrawal symptoms. This double action makes fentanyl more addictive than other opioids. People use it to chase the high and escape withdrawal.
Research identifies four ways fentanyl hooks users:
- Positive reinforcement: Euphoric effects from dopamine release create powerful reward signals the brain seeks to repeat
- Negative reinforcement: Withdrawal symptoms including anxiety and physical discomfort compel continued use
- Tolerance: Repeated exposure requires increasing doses to achieve the same effects
- Physical dependence: Body systems adjust to function with fentanyl present, triggering withdrawal when use stops
Genetics play a role through incentive sensitization. Repeated fentanyl use makes reward pathways hypersensitive to anything associated with the drug.
How Does Fentanyl Compare to Heroin?
Both fentanyl and heroin are opioids, but fentanyl is far more potent and addictive. Fentanyl’s extreme potency makes it deadlier than heroin in distinct ways.
- Potency: Fentanyl is 50 times stronger than heroin
- Overdose risk: Higher with fentanyl due to extreme potency; respiratory depression occurs more rapidly
- Addiction mechanism: Fentanyl engages both positive and negative reinforcement pathways simultaneously
- Detection: Fentanyl is often mixed into heroin without user knowledge
- Speed of action: Fentanyl acts faster, increasing risk of sudden respiratory failure
Fentanyl-laced heroin has completely reshaped the overdose crisis. Many people buying heroin get fentanyl instead, or mixed in, without knowing it.
What are the Symptoms of a Fentanyl Overdose?
Fentanyl overdose happens when the drug shuts down breathing to life-threatening levels. Spotting these symptoms fast can mean the difference between life and death.
- Pinpoint pupils (extremely small)
- Slow, shallow, or stopped breathing
- Blue lips or fingernails
- Cold, clammy skin
- Limp, unresponsive body
- Call 911 immediately
- Administer naloxone (Narcan) if available
- Perform rescue breathing if trained
- Place person on their side to prevent choking
Withdrawal hits when someone physically dependent on fentanyl stops using. Symptoms usually start within 12 hours of the last dose. Expect muscle pain, chills, nausea, anxiety, and crushing cravings. These symptoms feel unbearable, but they’re temporary, and manageable with medical support.
Trying to detox alone is risky. Withdrawal can be severe, and relapse rates are high without medical support. Medical detox programs offer round-the-clock monitoring and FDA-approved medications (methadone, buprenorphine, naltrexone) to ease symptoms safely.
Fentanyl-laced heroin and fake pills expose users to a dangerously potent drug, often without their knowledge. Most people buying drugs don’t expect fentanyl to be in what they’re getting. This unpredictability has sent fatal overdoses soaring among people who thought they were using safer drugs.
Fake pills that look like real oxycodone or Xanax now routinely contain fentanyl. Users can’t tell what’s actually in these pills or how strong they are. Every use could be fatal.
Fentanyl Abuse and Co-Occurring Disorders
Fentanyl addiction rarely happens alone. Most people who become dependent on fentanyl also struggle with mental health issues. SAMHSA’s 2024 data shows that about 37% of people with opioid use disorder also have at least one mental health condition.
Common mental health conditions that accompany fentanyl addiction include:
- Anxiety disorders: Fentanyl triggers receptors in the central amygdala, ramping up fear responses during withdrawal
- Depression: People dealing with depression often turn to fentanyl to escape emotional pain, even if just temporarily
- PTSD: Trauma survivors frequently use opioids to numb intrusive memories and emotional pain
Treating addiction without addressing mental health usually leads to relapse. At Peak Path Health, our dual diagnosis treatment tackles both fentanyl addiction and co-occurring mental health conditions.
Fentanyl Addiction FAQs
Fentanyl addiction can develop fast because of how potent it is. Some people become dependent after just a few uses. Your brain starts adapting to fentanyl within days. Physical dependence can set in within one to two weeks of regular use.
Yes. Comprehensive programs that combine medical detox, therapy, and ongoing support can successfully treat fentanyl addiction. Treatment tackles both physical dependence and the brain changes fentanyl causes, using medications and proven therapies.
Fentanyl is 50 to 100 times stronger than morphine. It activates two brain pathways at once, triggering intense euphoria and brutal withdrawal. This double action makes it more addictive than other opioids.
Research shows genetics play a major role in fentanyl addiction vulnerability. A family history of addiction increases your risk through inherited traits that affect how your brain responds to opioids.
Help for Fentanyl Addiction is Available
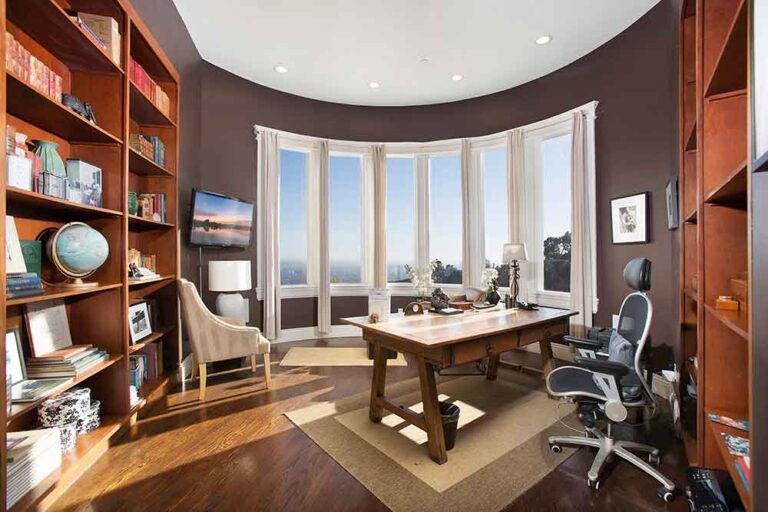
Recovering from fentanyl addiction takes comprehensive treatment that addresses physical dependence and the complex ways the drug rewires your brain. Peak Path Health offers specialized care to support you through every stage of healing at our luxury facilities in the Hollywood Hills and Woodland Hills neighborhoods of Los Angeles.
Medical detox is the critical first step. You’ll get 24-hour supervision and FDA-approved medications to manage withdrawal safely. Residential treatment blends evidence-based therapies, individual sessions, group work, Cognitive Behavioral Therapy, with holistic approaches like yoga, meditation, and art therapy. You’ll also enjoy chef-prepared meals, massage therapy, and peaceful outdoor spaces for exercise and reflection.
With the right professional support, recovery is within reach. If you or someone you love is struggling with fentanyl, reach out to Peak Path Health today. Recovery starts here.