As temperatures drop and daylight hours shorten, many people notice shifts not only in the weather but also in their mental and emotional well-being. For people struggling with mental health conditions or substance use disorders, fall and winter can be particularly challenging seasons. Across the United States, and especially in fast-paced urban areas such as Los Angeles, California, treatment centers often see an increase in people seeking help during these colder, darker months.
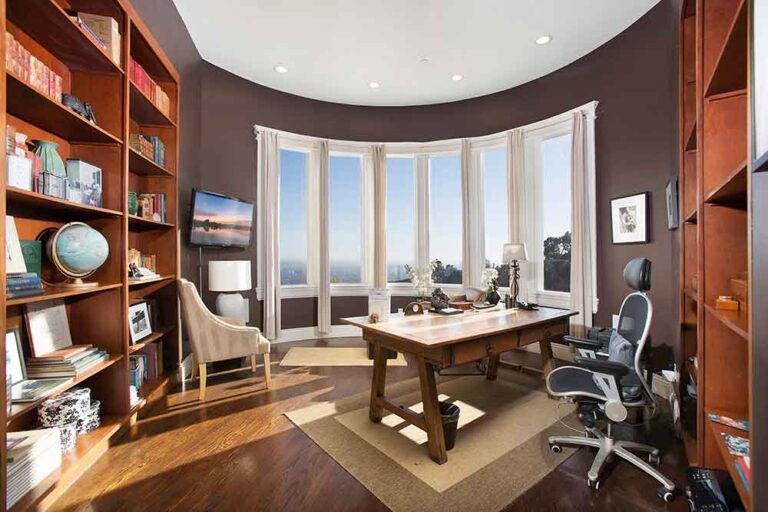
At Peak Path Health, serving individuals in Hollywood Hills and Woodland Hills of Los Angeles, CA, clinicians regularly observe this seasonal pattern. While winter is often associated with holidays, connection, and reflection, it can also intensify feelings of loneliness, depression, anxiety, and substance use. Understanding why more people seek addiction and mental health treatment during fall and winter can help normalize these experiences and encourage earlier, healthier support.
What Is Seasonal Depression?
Seasonal depression refers to mood changes that occur during specific times of the year, most commonly in fall and winter. These changes are often linked to reduced sunlight, disrupted sleep cycles, and shifts in daily routines. While not everyone experiences clinical depression during winter months, many people report feeling more fatigued, withdrawn, and emotionally vulnerable.
The Psychological Impact of the Winter Blues
Shorter days and longer nights can significantly affect brain chemistry. Reduced sunlight exposure impacts serotonin levels, a neurotransmitter responsible for mood regulation, and disrupts melatonin production, which influences sleep patterns. These biological shifts can lead to:
- Persistent low mood
- Increased fatigue and sluggishness
- Difficulty concentrating
- Reduced motivation
- Social withdrawal
In cities like Los Angeles, where sunshine is typically abundant, even subtle seasonal changes can feel disruptive, especially for individuals already managing mental health or substance use challenges.
The Winter Blues vs Seasonal Affective Disorder
While the terms “winter blues” and “seasonal depression” are often used interchangeably, there are important distinctions between temporary seasonal mood changes and clinical conditions.
What Are the Winter Blues?
The winter blues describe mild, temporary mood changes that occur during colder months. Symptoms may include low energy, irritability, or a desire to stay indoors more often. While uncomfortable, winter blues generally do not interfere significantly with daily functioning and tend to improve as seasons change or routines stabilize.
What Is Seasonal Affective Disorder (SAD)?
Seasonal affective disorder (SAD) is a form of major depressive disorder with a seasonal pattern. According to the National Institute of Mental Health, SAD symptoms typically emerge in late fall or early winter and resolve in spring or summer. Unlike the winter blues, SAD can severely impact a person’s ability to function.
Common SAD symptoms include:
- Persistent sadness or hopelessness
- Loss of interest in previously enjoyed activities
- Changes in appetite or weight
- Sleep disturbances (oversleeping or insomnia)
- Difficulty concentrating
- Feelings of worthlessness
Without treatment, people are at an increased risk of seasonal affective disorder and addiction, along with relapse and mental health challenges.
Why Fall & Winter Are When People Seek the Most Help
Mental health professionals consistently report higher treatment admissions during the fall and winter months. Several factors contribute to this seasonal trend.
Fall often marks a natural transition period. The end of summer, return to routines, and approaching year-end can prompt reflection. Many individuals begin to evaluate their mental health, relationships, and coping habits more honestly during this time.
Summer months are often filled with social activities, travel, and extended daylight that can temporarily mask underlying struggles. When life slows down in fall and winter, unresolved emotional pain and substance use patterns become harder to ignore.
The holiday season can intensify feelings of grief, loneliness, family conflict, or unmet expectations. For individuals with a history of addiction or mental health disorders, these emotional pressures can surface old patterns and prompt the realization that professional help is needed.
Fall and winter often align with changes in insurance coverage, work schedules, and family availability, making it easier for people to commit to treatment during these months.
SAD Symptoms and Self-Medicating
One of the most concerning aspects of seasonal depression is the increased likelihood of self-medicating behaviors.
The Risks of Self-Medicating During the Winter Blues
Self-medicating involves using substances, such as alcohol, prescription medications, or illicit drugs, to cope with emotional distress. During winter months, individuals may turn to substances to manage symptoms like low mood, anxiety, insomnia, or social discomfort.
While substances may provide temporary relief, they often worsen depressive symptoms over time and increase dependence. Alcohol, for example, is a central nervous system depressant that can intensify feelings of sadness and fatigue while disrupting sleep.
The Link Between Seasonal Affective Disorder and Addiction
Seasonal mood changes and substance use disorders are closely linked. Research shows that individuals experiencing depression, seasonal or otherwise, are at a higher risk of developing or relapsing into substance use disorders.
How Winter Blues Contribute to Substance Use
Several mechanisms explain this connection:
- Mood regulation: Substances may be used to artificially elevate mood or numb emotional pain.
- Social isolation: Increased isolation during winter can reduce accountability and support.
- Sleep disruption: Insomnia or oversleeping may lead individuals to misuse substances to regulate rest.
- Lower motivation: Reduced energy can make healthy coping strategies feel overwhelming.
In Los Angeles, where social connection and productivity are often emphasized year-round, individuals may feel added pressure to “push through” emotional struggles, sometimes by turning to substances instead of support.
Risk Factors Connected to Addiction During Winter
Winter months introduce unique risk factors that can increase substance use and overdose rates.
Drug Overdoses: Why Do They Increase in Winter?
Public health data consistently shows an increase in overdose deaths during colder months. Contributing factors include:
- Using substances alone due to isolation
- Changes in tolerance following periods of reduced use
- More potent drug supplies
- Delayed emergency response times during winter weather
- Increased depression and hopelessness
Cold weather also increases physiological stress on the body, making an overdose more dangerous and recovery more difficult.
Coping With the Winter Holiday Pressures
While holidays are often portrayed as joyful, they can be emotionally complex, especially for individuals in recovery or those struggling with mental health.
Winter and Mental Health
Common winter stressors include:
- Family conflict or estrangement
- Financial pressure
- Grief and loss
- Unrealistic social expectations
- Increased isolation
These pressures can exacerbate depression and anxiety, increasing the urge to escape through substances.
How to Cope With Winter Blues Without Turning to Substances
Healthy coping strategies are essential during the fall and winter months. While professional support is often necessary, small daily changes can also help stabilize mood.
Effective coping strategies include:
- Maintaining routine: Regular sleep, meals, and movement help regulate mood
- Light exposure: Spending time outdoors or using light therapy can support serotonin levels
- Physical activity: Even gentle movement improves energy and emotional regulation
- Social connection: Staying connected reduces isolation and relapse risk
- Mindfulness and therapy: Learning to sit with discomfort rather than escape it
At Peak Path Health, clinicians help individuals build personalized coping plans that support long-term stability, not just seasonal relief.
Treatment for Seasonal Affective Disorder and Addiction
Seasonal depression is highly treatable, especially when addressed early. Comprehensive treatment addresses both mood symptoms and any co-occurring substance use. At Peak Path Health in Hollywood Hills and Woodland Hills, residential and structured outpatient services are designed to address the emotional, psychological, and behavioral components of seasonal affective disorder and addiction.
Treatment plans may include cognitive behavioral therapy (CBT), trauma-informed care, relapse prevention planning, and lifestyle stabilization, all essential for navigating seasonal challenges.
For individuals experiencing severe depression, relapse risk, or co-occurring disorders, residential treatment provides structured, immersive support. Residential care offers:
- 24/7 clinical supervision
- Integrated mental health and addiction treatment
- Individual therapy and group therapy
- Medication management
- Holistic therapy
Dual diagnosis treatment addresses both mental health conditions and substance use disorders at the same time, recognizing how closely they are connected. By treating conditions such as seasonal affective disorder and addiction together, individuals receive more effective, coordinated care that reduces relapse risk and supports long-term stability. This integrated approach helps people build healthier coping skills while addressing the underlying causes of both conditions.
Start Recovery Today: We’re Here for You
If fall or winter has intensified feelings of depression, isolation, or substance use, you are not alone, and you don’t have to wait for spring to feel better. Seasonal struggles are real, valid, and treatable.
Peak Path Health provides compassionate, evidence-based mental health and addiction treatment for adults in Los Angeles, with locations serving Hollywood Hills and Woodland Hills. Whether you’re experiencing seasonal depression, substance use concerns, or both, our team is here to help you build a healthier path forward.
Recovery doesn’t have a season. Reach out today to learn how Peak Path Health can support you through winter and beyond.