Seasonal depression affects approximately 5% of adults in the United States each year. That’s roughly 16 million people struggling with more than just the winter blues. Unlike temporary winter blues, seasonal affective disorder (SAD) is a diagnosable mental health condition that can derail your work, strain your relationships, and leave you unable to get through basic daily tasks.
According to research published by the National Institutes of Health, seasonal depression has a substantial genetic component. Twin studies show that genetic factors account for at least 29% of the variance in seasonal mood patterns. Family studies demonstrate that relatives of people with SAD have rates of the disorder ranging from 14-26%, indicating a clear hereditary influence.
Scientists have identified specific genes involved in circadian rhythm regulation that contribute to seasonal depression risk. This genetic basis explains why winter depression often runs in families, showing up generation after generation. Peak Path Health’s depression treatment center in Los Angeles, California, addresses both the biology behind seasonal depression and the environmental triggers that make it worse.
How Do the Winter Blues Impact Those in Recovery?
Winter blues refer to mild seasonal mood changes, while seasonal affective disorder represents a clinically diagnosed form of depression. People in recovery face a tougher battle during the winter months. Seasonal changes can trigger both cravings and mood swings that threaten sobriety.
Key differences between winter blues and SAD:
- Duration: Winter blues are temporary; SAD persists for months
- Severity: SAD significantly impairs daily functioning
- Treatment needs: SAD requires professional intervention
Seasonal Changes Can Affect Our Mood
Weather and seasonal changes affect mood in clear, biological ways. Reduced sunlight during shorter days disrupts circadian rhythms, the internal clock that regulates sleep, hormones, and body temperature. When this system is thrown off, neurotransmitter balance is affected, especially serotonin, which plays a key role in mood stability.
Studies show that decreased daylight can lower serotonin production by as much as 25% in vulnerable individuals, increasing the risk of depressive symptoms. Because the body’s internal clock depends on light cues, disrupted rhythms can lead to sleep disturbances, low energy, and emotional instability.
Weather-related changes in brain chemistry include:
- Melatonin production: Altered by sunlight, affecting sleep quality and timing
- Vitamin D synthesis: Often reduced in winter and linked to mood regulation
- Circadian rhythm genes: Influence how sensitive individuals are to seasonal light changes
Understanding how seasonal changes affect brain chemistry highlights why mood shifts during certain times of year are not a personal failure, but a biological response. When light exposure, sleep patterns, and neurotransmitter balance are disrupted, mental health can suffer, especially for those already vulnerable to depression or substance use. With the right support, structure, and treatment, these seasonal effects can be managed, helping restore emotional balance and protect long-term well-being.
Winter Blues Vs Seasonal Affective Disorder

Winter blues are temporary mood dips during colder, darker months. Unlike clinical depression, these shifts lift naturally in spring and typically don’t interfere with work, relationships, or daily responsibilities. Most people experience minor, manageable mood changes related to weather or reduced daylight.
Seasonal Affective Disorder (SAD), on the other hand, is a form of depression that recurs at specific times of the year, usually fall and winter, when daylight hours are shorter. According to the National Institute of Mental Health, SAD affects about 5% of U.S. adults, with higher rates in northern regions. A diagnosis requires depressive symptoms to appear in the same season for at least two consecutive years and improve when the season changes. A family history of SAD also increases the risk.
What Comes First, Depression or Substance Abuse?
Seasonal depression and substance abuse frequently co-occur, with some individuals using alcohol or drugs to manage depressive symptoms during darker months. This pattern of self-medication makes both conditions worse instead of providing any real relief.
Treating both seasonal depression and addiction at the same time works better than tackling them separately, especially since genetics accounts for 40-60% of the risk for both conditions when they run in families.
Signs and Symptoms of Seasonal Affective Disorder
Seasonal depression symptoms typically emerge in late fall or early winter and last at least two weeks, making daily functioning difficult. It often appears as persistent sadness, loss of interest in activities, and noticeable changes in sleep and appetite.
Winter depression has a distinct pattern that follows the seasons and includes physical symptoms not common in other types of depression. People with seasonal affective disorder (SAD) often crave carbohydrates, gain weight, and sleep more, unlike the insomnia seen in major depression. Key symptoms include:
- Emotional: Sadness, hopelessness, irritability, anxiety
- Physical: Fatigue, weight gain, oversleeping, carbohydrate cravings
- Behavioral: Social withdrawal, difficulty concentrating, reduced productivity
With awareness and proper support, seasonal depression can be managed, helping you maintain mood, energy, and daily functioning throughout the winter months.
Who is at Risk for Seasonal Depression?
Seasonal depression doesn’t affect everyone equally. Certain groups face a much higher risk. Women develop seasonal affective disorder four times more than men. Young adults between 18 and 30 are most likely to develop SAD for the first time.
Where you live matters when it comes to seasonal depression risk. People living in northern latitudes with reduced winter sunlight face higher rates of SAD compared to those in southern regions. The farther you live from the equator, the more dramatic the seasonal light changes you’ll experience. Risk factors include:
- Gender: Women develop SAD at rates four times higher than men
- Age: Most common onset occurs between ages 18 and 30
- Geography: Northern latitudes with limited winter sunlight show a higher prevalence
- Family history: Genetic effects account for 29% of the variance in seasonality
- Mental health history: Previous depression or bipolar disorder increases risk
Understanding who is at risk for seasonal depression can help you recognize early signs and seek support before symptoms interfere with your daily life.
Is Seasonal Depression Genetic?
Seasonal depression does have a significant genetic component. Research from the National Institutes of Health shows that twin studies attribute at least 29% of differences in seasonality and mood changes to genetics. Family studies also indicate that individuals with a parent who has seasonal affective disorder (SAD) are more likely to develop the condition themselves. Overall, SAD appears to follow a complex inheritance pattern, with 14–26% of relatives affected, far higher than rates seen in the general population.
Scientists have also identified three core clock genes that influence vulnerability to seasonal affective disorder.
- Genome-wide association studies show this gene has the strongest link to SAD, regulating circadian rhythms, sleep, hormone release, and mood.
- Variants increase sensitivity to daylight changes
- Affects serotonin and other neurotransmitter pathways
- Maintains internal clock and sleep timing
- Variants linked to seasonal mood changes
- Disruptions impact sleep, energy, and circadian stability
- Master circadian regulator, partners with NPAS2
- Variants affect light sensitivity and mood
- Controls melatonin, serotonin, and other circadian genes
- The first human gene mutation directly connected to increasing the risk of SAD.
- Regulates sleep-wake timing and circadian rhythm
- Alters sleep and hormone cycles, heightening winter mood changes
Certain genetic combinations increase the risk of seasonal affective disorder by four to ten times. These genes influence how the brain responds to changes in light and seasonal shifts.
Seasonal Depression and Addiction: What’s the Connection?
Seasonal depression and substance use disorders often occur together, making recovery more challenging. The National Institute on Drug Abuse reports that people with mood disorders, including seasonal affective disorder (SAD), are about twice as likely to develop a substance use disorder as the general population.
Winter months can increase this vulnerability. Shorter days, colder weather, and disrupted routines can negatively affect mood, energy, and daily functioning, making substances like alcohol more tempting as a coping mechanism. Alcohol may temporarily relieve fatigue or low mood, but it disrupts the same serotonin and dopamine systems already affected by seasonal depression. Over time, this creates a self-reinforcing cycle: substance use worsens depressive symptoms, and depression drives more substance use.
Reduced sunlight lowers serotonin levels and interferes with circadian rhythms, contributing to fatigue, sleep disturbances, and low motivation. Social isolation from colder weather and fewer activities can lead to loneliness, boredom, and time spent alone, factors closely linked to substance misuse. For individuals in recovery, the loss of structure and support during winter can weaken coping skills and increase relapse risk.
Seasonal stressors, such as holiday pressures, family conflict, and year-end grief or reflection, can intensify emotional distress. Combined with limited access to healthy coping outlets like exercise or social connection, these factors raise the likelihood of developing a substance use disorder or experiencing escalation of existing use.
Tips for Battling Seasonal Depression
Managing winter depression during recovery means combining proven treatments with consistent daily routines. Light therapy is a primary treatment. Research shows that 30 minutes of 10,000 lux exposure each morning helps regulate the circadian rhythm genes involved in seasonal depression.
Sleep consistency is especially important if you’re genetically predisposed to seasonal depression. Disruptions in your sleep-wake cycle can trigger mood episodes. Sticking to fixed bedtime and wake times helps keep your circadian rhythm stable. Effective strategies include:
- Light therapy: 10,000 lux light box for 30 minutes daily
- Exercise routine: Regular physical activity, especially outdoors
- Sleep hygiene: Consistent bedtime and wake times
- Social connection: Maintaining contact with support networks
- Professional support: Regular therapy and medication management
How to Beat the Winter Blues and Maintain Sobriety
Staying sober during the winter months takes preparation, especially if you’re genetically predisposed to seasonal depression. People in recovery can build resilience by developing winter-specific strategies before symptoms typically show up in late fall.
This means increasing therapy sessions during vulnerable months, finding sober winter activities, and having a solid plan for managing cravings when they hit. Dual diagnosis programs tackle both seasonal depression and substance use disorders at the same time, knowing that genetic predisposition to seasonal mood changes can make recovery harder.
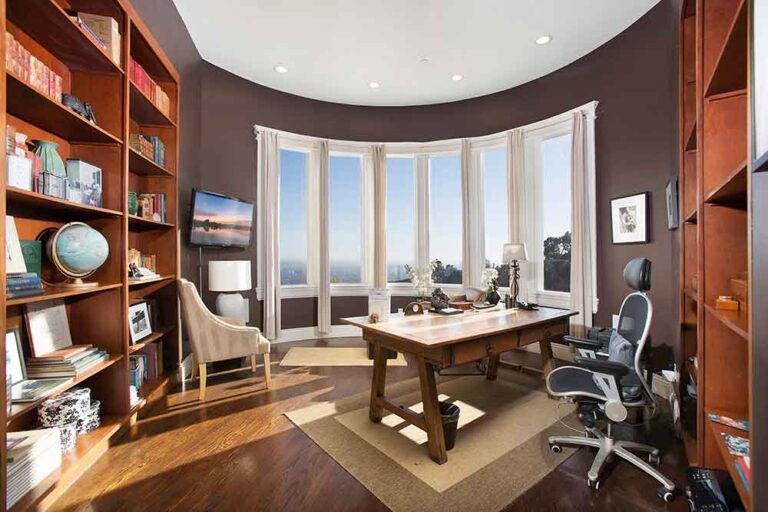
You’re Not Alone at Peak Path Health
We understand the complex relationship between seasonal depression and substance use disorders. At Peak Path Health in Hollywood Hills and Woodland Hills of Los Angeles, CA, specialized dual diagnosis treatment addresses both conditions simultaneously, providing the tools, structure, and support needed for long-term recovery and emotional stability.
When seasonal depression and substance use co-occur, shared genetic factors often play a role. Understanding each client’s genetic and clinical background helps inform a personalized treatment plan tailored to their unique needs.
If seasonal depression is impacting your recovery or occurring alongside substance use, you don’t have to face it alone. Contact Peak Path Health today to begin recovery with care designed around you.