Anxiety and addiction often appear together, creating unique challenges for those affected. At Peak Path Health, we understand how these two conditions can reinforce each other, making recovery more complex. Our team specializes in addressing both issues simultaneously, providing comprehensive dual diagnosis treatment that acknowledges the connection between anxiety symptoms and substance use.
When anxiety and addiction occur together, they can create a cycle that’s difficult to break without professional help. Many people use substances to temporarily relieve anxiety symptoms, only to find their anxiety worsens over time. Understanding this relationship is the first step toward effective treatment.
Recent statistics from the Substance Abuse and Mental Health Services Administration (SAMHSA) show that approximately 9.2 million adults in the United States experience both mental illness and substance use disorders. This highlights how common these co-occurring conditions are and the importance of specialized treatment programs.
Addiction, or substance use disorder, is characterized by continued use of substances despite harmful consequences. It involves changes in brain function that make stopping difficult, even when a person wants to quit. The American Psychiatric Association defines addiction as a complex condition affecting brain function and behavior, emphasizing the need for comprehensive substance use disorder treatment.
When these conditions occur together, healthcare professionals refer to them as co-occurring disorders or dual diagnosis. This means a person experiences both a mental health condition (anxiety) and a substance use disorder simultaneously. The relationship between these conditions is often complex and bidirectional.

Prevalence of Anxiety Disorders and Addiction
Different anxiety disorders show varying rates of substance use. For instance, social anxiety disorder has particularly high rates of alcohol use disorder, while panic disorder shows stronger associations with prescription medication misuse. Generalized anxiety disorder (GAD) appears alongside a wide range of substance use patterns. Key facts about co-occurring anxiety and addiction include:
- Anxiety disorders affect approximately 19.1% of adults in the United States annually.
- Substance Use Disorders impact roughly 14.8% of adults aged 18 or older
- Co-occurrence Rate: About 18% of people with anxiety disorders also have substance use disorders
Age plays a role in these patterns as well. Young adults (ages 18-25) show the highest rates of co-occurring anxiety and substance use. This age group is particularly vulnerable as they navigate major life transitions while their brains are still developing, and residential addiction treatment in Los Angeles can offer vital support.
The COVID-19 pandemic significantly increased rates of both anxiety and substance use. A 2021 study published in JAMA Psychiatry found a 25% increase in anxiety disorders globally during the pandemic, while substance use rates rose by similar margins.

Why Does Anxiety and Addiction Co-Occur?
Many people with anxiety use substances to reduce their symptoms. This is called self-medication. For example, someone with social anxiety might drink alcohol to feel more comfortable in social situations. While this may provide temporary relief, it often leads to a harmful cycle:
- Anxiety symptoms become uncomfortable
- Substance use temporarily reduces anxiety
- The brain begins to rely on substances for relief
- Tolerance develops, requiring more of the substance
- Stopping causes anxiety to worsen (rebound anxiety)
- The person uses it again to avoid discomfort
Research from the National Institute on Mental Health shows that alcohol and certain drugs affect the same brain systems that regulate anxiety. This explains why the relief is temporary and often leads to worse anxiety over time.
Anxiety and addiction share common biological factors. Both conditions involve similar brain regions and neurotransmitter systems, including:
- The amygdala (processes fear responses)
- The prefrontal cortex (handles decision-making)
- The GABA system (produces calming effects)
- The dopamine system (influences reward and motivation)
Genetic factors also play a role. Research suggests that certain genes may increase vulnerability to both anxiety and addiction. A family history of either condition raises the risk of developing both.
When someone who regularly uses substances tries to stop, withdrawal often includes intense anxiety symptoms. This happens because:
- The brain has adapted to the presence of the substance
- Natural anxiety regulation systems have become less effective
- Stress hormones increase during withdrawal
- The nervous system becomes hyperactive
This withdrawal-induced anxiety can be severe enough to drive continued substance use, creating another cycle that’s difficult to break without support.
Signs and Symptoms of Anxiety and Addiction
- Rapid heartbeat or palpitations
- Excessive sweating
- Trembling or shaking
- Sleep disturbances (insomnia or oversleeping)
- Digestive problems
- Fatigue or low energy
- Changes in weight or appetite
- Avoiding social situations or responsibilities
- Using substances before anxiety-provoking events
- Increased secrecy or lying about substance use
- Changes in friend groups or activities
- Declining performance at work or school
- Financial problems related to substance purchases
- Persistent worry or fear
- Difficulty concentrating
- Irritability or mood swings
- Feeling on edge or restless
- Racing thoughts
- Panic attacks
- Strong cravings for substances
The specific symptoms may vary depending on the type of anxiety disorder and substances used. For example, someone with panic disorder who uses depressants like alcohol might show different symptoms than someone with generalized anxiety who uses stimulants.


Risk Factors Linking Anxiety and Drug Use
Research from the National Institute on Drug Abuse indicates that genetics accounts for approximately 40-60% of addiction risk. Similarly, anxiety disorders show significant heritability (30-50%). Some genetic factors appear to influence both conditions.
Having close family members with either anxiety disorders or substance use problems increases personal risk. This may be due to both shared genetic traits and learned behaviors within families.
Experiencing trauma, especially during childhood, significantly increases risk for both anxiety and addiction. Adverse childhood experiences (ACEs) such as abuse, neglect, or household dysfunction can alter brain development in ways that affect stress response systems.
According to the Centers for Disease Control and Prevention (CDC), people with four or more ACEs are:
- 2-4 times more likely to develop anxiety disorders
- 5-7 times more likely to develop substance use disorders
- 10-12 times more likely to experience both conditions together
Ongoing stress from factors like poverty, discrimination, or unsafe living conditions also contributes to this risk.
Other mental health conditions often appear alongside anxiety and addiction, creating more complex clinical pictures. Depression is particularly common, with about 20% of people with anxiety disorders also experiencing major depression, highlighting the value of a depression treatment center for comprehensive care.
Attention-deficit/hyperactivity disorder (ADHD), post-traumatic stress disorder (PTSD), and certain personality disorders also frequently co-occur with anxiety and substance use. Each additional condition can complicate treatment and recovery.
Treating Addiction and Anxiety Disorder with an Integrated Approach
- Comprehensive assessment of both conditions
- Treatment planning that addresses both anxiety and substance use
- Coordination between mental health and addiction specialists
- Therapies that target shared underlying factors
- Medications are carefully selected to avoid triggering either condition
Research published in the Journal of the American Medical Association shows that integrated treatment leads to better outcomes than sequential treatment (treating one condition first, then the other) or parallel treatment (treating both conditions but through separate, uncoordinated systems).
At Peak Path Health, our integrated approach ensures clients receive care from a team that understands the complex relationship between anxiety and addiction. Our personalized anxiety treatment in Hollywood, California, address both conditions from the start, with regular adjustments based on individual progress.
Anxiety and Addiction Treatment
Cognitive Behavioral Therapy (CBT) is highly effective for both anxiety disorders and substance use disorders. This structured approach helps identify and change unhelpful thought patterns and behaviors that maintain both conditions, and cognitive behavioral therapy is often recommended for individuals requiring comprehensive intervention. In CBT sessions, clients learn to:
- Recognize anxiety triggers and high-risk situations for substance use
- Challenge distorted thinking that contributes to anxiety and cravings
- Develop healthy coping strategies to replace substance use
- Practice gradual exposure to anxiety-provoking situations
- Create relapse prevention plans that address both conditions
Research shows CBT can reduce anxiety symptoms by 50-80% while significantly decreasing substance use. The skills learned in CBT continue to benefit people long after formal treatment ends.
Family therapy can help address relationship patterns that might unintentionally maintain anxiety or substance use. These sessions provide safe spaces to improve communication, set healthy boundaries, and rebuild trust.
Certain medications can help manage anxiety symptoms without creating new risks for substance use. These medications are carefully selected based on a person’s specific anxiety disorder, substance use history, and other health factors. Common medications used to treat anxiety and addiction may include:
- Selective serotonin reuptake inhibitors (SSRIs) like sertraline or escitalopram
- Serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine
- Buspirone, which treats anxiety without sedative effects
- Naltrexone for alcohol or opioid use disorders
- Acamprosate for alcohol use disorder
- Buprenorphine for opioid use disorder
Medication decisions always consider the risk of cross-addiction or interactions. Regular monitoring ensures medications remain effective without creating new problems.
Mindfulness practices help people develop awareness of their thoughts, feelings, and physical sensations without judgment. These techniques can reduce anxiety while building resilience against cravings. Evidence-based mindfulness approaches include:
- Mindfulness-Based Relapse Prevention (MBRP)
- Mindfulness-Based Stress Reduction (MBSR)
- Yoga and meditation practices
- Breathwork
- Deep breathing exercises
- Progressive muscle relaxation
- Guided imagery
- Journaling
- Stress management and boundary-setting
- Connecting with supportive people
Recovery from co-occurring anxiety and addiction extends beyond addressing immediate symptoms. A holistic approach supports whole-person healing and sustainable wellness. Learning to manage stress effectively is essential for long-term recovery. These skills help people navigate life challenges without turning to substances or becoming overwhelmed by anxiety. Mindfulness practices can be as effective as medication for certain anxiety disorders while also supporting addiction recovery.
Diet and exercise significantly impact both anxiety and addiction recovery. Nutritional approaches focus on:
- Stabilizing blood sugar to reduce anxiety fluctuations
- Providing nutrients that support brain health (omega-3s, B vitamins)
- Repairing nutritional deficiencies common in addiction
- Establishing regular eating patterns
Regular physical activity reduces anxiety symptoms through several mechanisms:
- Releasing endorphins that improve mood
- Reducing stress hormones like cortisol
- Improving sleep quality
- Building confidence and body awareness
- Providing a healthy structure and routine
Even moderate activities like walking, swimming, or gentle yoga can provide significant benefits for both conditions.
Recovery is an ongoing process that extends beyond formal treatment. Continuing care might include:
- Step-down levels of treatment (from residential to outpatient)
- Regular check-ins with treatment providers
- Participation in support groups
- Booster therapy sessions during high-stress periods
- Ongoing medication management if needed
Research shows that longer engagement with recovery support correlates with better outcomes for both anxiety and addiction.


Anxiety and Addiction Treatment FAQs
Treatment costs vary based on level of care, location, and insurance coverage. Residential treatment typically ranges from $20,000-$65,000 per month, while outpatient programs may cost $5,000-$10,000 per month. Many insurance plans cover a significant portion of these costs.
The initial assessment includes a comprehensive evaluation of mental health symptoms, substance use patterns, medical history, and personal goals. This process typically involves interviews, questionnaires, and sometimes lab tests to develop a personalized treatment plan.
Recovery timelines vary widely depending on individual factors. Initial intensive treatment usually lasts 30-90 days, followed by ongoing support that may continue for months or years. Many people find that recovery becomes a lifelong journey of growth and maintenance.
Yes, certain medications can safely treat anxiety in people with a history. Non-addictive options like SSRIs, SNRIs, and buspirone are commonly prescribed. Medication decisions should always involve open discussion about addiction concerns and close monitoring by healthcare providers.
Begin Your Personalized Recovery Journey
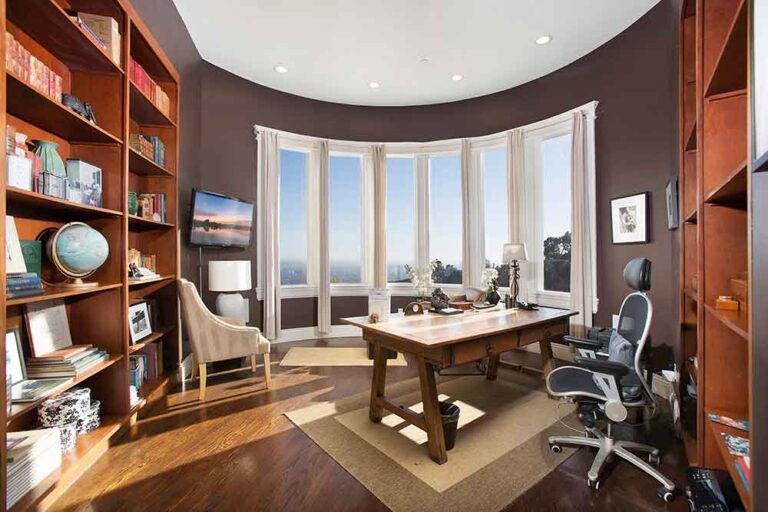
Located in the Hollywood Hills, our center offers a peaceful environment where clients can focus fully on healing. Our expert team includes specialists in both mental health and addiction medicine who work together to create truly personalized treatment plans.
If you or someone you care about is struggling with anxiety and addiction, we’re here to help. Recovery is possible with the right support.