OCD and addiction are two conditions that can occur separately or together. When they appear at the same time, they create unique challenges that require specialized treatment. At Peak Path Health in the Hollywood Hills and Woodllan Hills of Los Angeles, California, dual diagnosis residential treatment addresses both conditions simultaneously, helping individuals break the cycle of intrusive thoughts, compulsive behaviors, and substance use.
Living with OCD involves unwanted thoughts and repetitive behaviors aimed at reducing anxiety. When combined with addiction, substances may temporarily ease these symptoms but ultimately worsen the condition. Our luxury drug rehab center offers a peaceful environment where patients can focus on recovery through evidence-based treatment programs, medication management, and holistic therapy.
OCD can profoundly disrupt daily life, relationships, and overall well-being. Although individuals with OCD often recognize that their thoughts and behaviors are excessive or irrational, they may feel unable to control them. This can lead to harmful coping strategies, including developing bad habits, making poor decisions, or self-medicating with drugs or alcohol. Without treatment, serious social, psychological, and physical consequences often arise. Effective care typically combines therapy with medication when needed to manage symptoms and support long-term recovery.


The Link Between OCD and Addiction
About 27% of individuals with OCD develop a substance use disorder, significantly higher than the general population. Both conditions involve changes in brain circuits that shift behavior from goal-directed to habitual, making actions difficult to control. Common features include repetitive behaviors, impaired control despite negative consequences, and interference with daily functioning and relationships.
Substance use may temporarily relieve OCD-related anxiety, but over time, it worsens both conditions, creating a cycle that is difficult to manage without integrated treatment. Addressing only one disorder often leads to limited improvement or a higher risk of relapse.
Signs and Symptoms of OCD and Addiction
- Work performance suffers due to time lost to both rituals and substance use
- Relationships become strained as people withdraw to hide symptoms or prioritize compulsions and substance use
- Self-care routines deteriorate, with basic hygiene or nutrition neglected
- Financial problems develop from spending on substances, while also potentially missing work due to OCD symptoms
For example, someone might be late to work repeatedly because their morning routine includes extensive checking rituals, followed by substance use to manage the resulting anxiety about being late. Also, someone may avoid social situations that trigger their OCD symptoms, then use substances when alone to cope with feelings of isolation.
This combined impact on functioning often exceeds what would be expected from either condition alone, creating a cycle where each disorder reinforces and worsens the other. Signs and symptoms of OCD and addiction include:
- Sudden weight changes, bloodshot eyes, trembling hands, or frequent nosebleeds
- Physical effects of OCD, such as raw or chapped hands from excessive washing
- Intense anxiety that shifts between obsessive thoughts and cravings
- Mood swings, shame, and guilt related to compulsions and substance use
- Social withdrawal and isolation to hide behaviors
Patterns of distress differ: OCD anxiety follows predictable thought-behavior cycles, while addiction-related anxiety often peaks during periods of abstinence.
- Nighttime rituals from OCD may delay sleep.
- Substance use can cause erratic sleep patterns, alternating between insomnia and oversleeping.
- Tremors, anxiety, or agitation from substance withdrawal may mimic OCD behaviors.
- Symptoms often appear during withdrawal rather than in response to specific triggers.
Recognizing these signs early is crucial for integrated treatment and lasting recovery.
OCD and Addiction Treatment at Peak Path Health
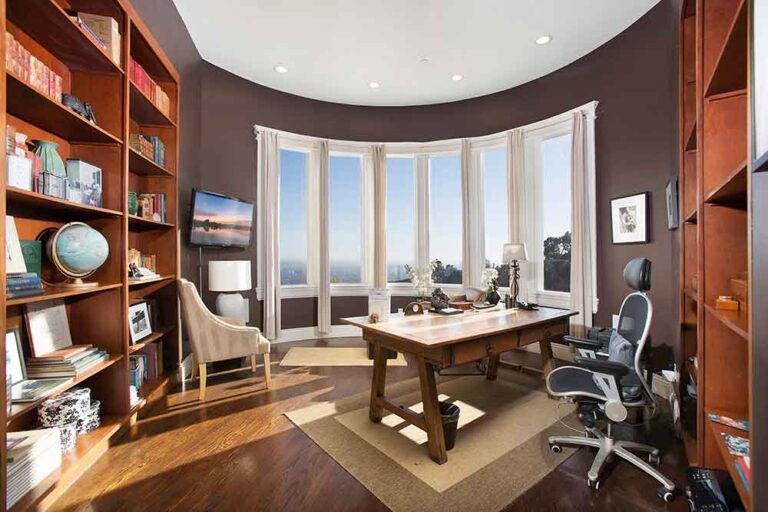
Through structured routines, compassionate guidance, and proven therapeutic techniques, we help you build healthier coping skills and long-term stability. With holistic wellness services and dedicated clinical support, Peak Path Health’s luxury rehab in the Hollywood Hills and Woodland Hills offers a comprehensive luxury treatment experience focused on deep healing.
Patients benefit from private rooms, chef-prepared meals, yoga and meditation, massage, fitness facilities, outdoor recreation areas, and creative therapy spaces. A high staff-to-client ratio ensures attentive, individualized care and allows clinicians to closely observe how OCD and addiction interact. The serene environment, complete with nature, fresh air, and scenic views, reduces stress and supports recovery on both mental health and substance use levels.
Trauma-informed therapy recognizes the role past trauma can play in both OCD and addiction. Approaches such as Eye Movement Desensitization and Reprocessing (EMDR) help process traumatic memories that may contribute to symptoms, reducing their emotional impact and interrupting the cycle of anxiety and substance use. Peak Path Health provides integrated care for OCD and addiction, combining the following levels of care:
Medical detox is a critical first step in treating co-occurring OCD and addiction. At Peak Path Health, medications are carefully used to safely manage withdrawal symptoms and support the stabilization of both conditions. For OCD, selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help regulate serotonin levels, reducing obsessive thoughts and compulsive behaviors.
When OCD and addiction occur together, medication management becomes more complex. Our team of psychiatrists and addiction specialists works closely to monitor interactions, adjust dosages, and minimize side effects. This coordinated, individualized approach ensures that both conditions are addressed safely and effectively, laying the foundation for a successful recovery.
Residential treatment provides a structured environment where individuals can focus entirely on recovery from both OCD and addiction, a crucial option when choosing inpatient vs outpatient rehab. These programs typically include:
- 24-hour care and supervision
- Daily therapy sessions (individual and group)
- Medication management
- Structured daily routines
- Skills training for managing symptoms
- Peer support
California has specific licensing standards for facilities that treat co-occurring disorders. These include requirements for staff qualifications, treatment planning, and integrated care approaches. Facilities must demonstrate the ability to address both mental health and substance use simultaneously rather than treating them as separate issues.
Based on evaluations conducted, the clinical team develops an individualized treatment plan addressing both OCD and addiction. This plan includes specific therapy goals, medication options if appropriate, and strategies for managing symptoms of both conditions.
Peak Path Health utilizes a comprehensive, integrated approach to treating OCD and addiction, addressing how these conditions reinforce one another. Evidence-based therapies, including cognitive behavioral therapy (CBT), exposure and response prevention (ERP), and trauma-informed care, target the thoughts, triggers, and emotional patterns behind compulsions and substance use.
This cohesive approach helps reduce compulsions, manage cravings, and build healthier coping skills, supporting long-term stability and resilience. Additional therapies include acceptance and commitment therapy (ACT) to accept difficult thoughts and feelings, family therapy to improve relationships and support systems, and trauma-informed approaches such as eye movement desensitization and reprocessing therapy (EMDR) to process past trauma and break cycles of anxiety and substance use.
Cognitive behavioral therapy is highly effective for treating OCD and addiction together because it helps you understand how your thoughts, feelings, and behaviors contribute to both conditions, and gradually face fears without compulsions. Integrated CBT reduces OCD symptoms by 45% and substance use by 60%.
For OCD, a specialized CBT method called Exposure and Response Prevention (ERP) is especially beneficial. In ERP, you gradually face feared situations without performing rituals, such as touching a “contaminated” doorknob and resisting the urge to wash your hands, allowing anxiety to decrease naturally over time.
For addiction, CBT focuses on identifying triggers and developing healthier coping strategies. When used in an integrated way, CBT helps you recognize how OCD symptoms can fuel substance use and how substances may temporarily ease anxiety while ultimately making OCD worse.
Research supports this combined approach. The Journal of Behavior Therapy and Experimental Psychiatry reports that integrated CBT leads to a 45% reduction in OCD symptoms and a 60% reduction in substance use, outperforming treatments that address each condition separately.
Holistic therapies complement clinical treatment by addressing the physical, emotional, and spiritual aspects of recovery. These approaches help regulate the nervous system, reduce stress, and build healthy coping skills that support healing from both OCD and addiction. Mindfulness meditation increases awareness of thoughts without automatic reactions. This is especially valuable for OCD, where learning to observe intrusive thoughts without engaging in compulsions is essential. For addiction, mindfulness helps individuals recognize cravings without acting on them.
Yoga combines movement, breathwork, and meditation to reduce anxiety and improve body awareness. Research published in the Journal of Psychiatric Research shows that regular yoga practice can lower stress hormones and increase GABA, a neurotransmitter that promotes calm and reduces anxiety.
Nutritional therapy supports brain health during recovery. Both OCD and addiction can deplete key nutrients, and a balanced diet rich in omega-3 fatty acids, antioxidants, and complex carbohydrates supports healthy neurotransmitter production. Nutritional counseling helps individuals develop eating habits that strengthen recovery.
Why Personalized Care Matters
- Targeted interventions
- Flexible treatment pacing
- Trigger-specific support
- Customized coping strategies
Research shows that personalized care improves treatment completion rates and long-term outcomes for dual diagnosis patients.


Begin Your Healing Journey
Our luxury rehab center in the Hollywood Hills and Woodlaan Hills of Los Angeles, CA, offers the structure, support, and clinical expertise to help you break free from the cycle of compulsions and substance use. With personalized plans and a peaceful, healing environment, you gain the tools to understand your patterns, reduce distress, and develop lasting, healthy habits.
Whether you’re struggling with intrusive thoughts, compulsions, cravings, or all of these, you don’t have to face them alone. Our compassionate, evidence-based care team is here to guide you every step of the way.
If you’re ready to reclaim your life, Peak Path Health provides the private, tranquil setting you need. Your recovery starts now with one simple step. Contact us today to begin a journey toward strength, balance, and renewed hope.