Benzodiazepine addiction can develop even when these medications are taken as prescribed. For many individuals, what begins as a prescription for anxiety or insomnia gradually transforms into a dependency that’s difficult to break. Understanding the nature of benzodiazepine addiction is the first step toward recovery.
At Peak Path Health in Los Angeles, California, we recognize the complex challenges of benzodiazepine dependence. Our treatment programs address both the physical aspects of withdrawal and the psychological factors that contribute to continued use. As a result, clients can successfully overcome their challenges with drug addiction and maintain long-term sobriety.


Signs of Benzo Abuse
- Physical dependence: The body requires the drug to function normally
- Psychological reliance: Emotional attachment to the drug’s effects
- Loss of control: Inability to limit or stop use
- Continued use despite harm: Persisting despite negative consequences
Physical Indicators
Slurred speech may occur because benzos slow down brain activity. This can make it harder to form clear or coherent sentences.
Impaired coordination can look like stumbling or having trouble with balance. This happens because benzos affect areas of the brain that control motor function.
Memory problems may include forgetting recent events or struggling to follow conversations. These issues may become more noticeable over time.
Respiratory issues such as slowed breathing sometimes appear, especially when benzos are mixed with other depressants like alcohol or opioids. In such cases, professional opioid addiction treatment is often necessary for individuals with polysubstance use issues. This can be dangerous and is considered a medical emergency.
Withdrawal symptoms may show up when someone tries to stop taking benzos or reduce their dose. These can include anxiety, sweating, shaking, or even seizures, depending on the level of dependence.
Emotional and Behavioral Red Flags
Taking higher doses than prescribed without medical guidance may suggest tolerance. This happens when the current dose no longer has the same effect.
Spending significant time obtaining, using, or recovering from benzos can interfere with daily life. This might include planning activities around drug use or avoiding situations where benzos are not available.
Neglecting responsibilities might look like missing work, avoiding family obligations, or falling behind in school. These patterns often develop gradually.
Social withdrawal can involve pulling away from friends or family. Time spent alone may increase, especially if it is related to using or recovering from benzo use.
Mood swings or personality changes may appear as increased irritability, depression, or disinterest in things that used to matter. These changes may not always be recognized by the person experiencing them.
Why are Benzodiazepines Addictive?
This change in brain chemistry can lead to tolerance, where the brain gets used to the drug and the same dose no longer has the same effect. Over time, higher doses may be required to feel the same level of relief or sedation.
Even when used as prescribed, benzodiazepines can lead to physical dependence. Dependence occurs when the brain adapts to the ongoing presence of the drug, and withdrawal symptoms develop if the drug is stopped or reduced suddenly. Mechanisms of addiction include:
- Brain chemistry changes: Benzos increase GABA activity, which slows brain function and creates sedation. The brain may reduce its own GABA production in response.
- Reward pathway activation: Benzos can increase dopamine levels in the brain’s reward system. Dopamine is linked to feelings of pleasure, which can reinforce repeated use.
- Neuroadaptation: With consistent use, the brain adjusts to the presence of benzos. This makes it harder to function normally without the drug, increasing the risk of withdrawal and continued use.
Understanding Benzodiazepine Abuse Risks in California
California has seen shifts in benzo prescribing practices due to the ongoing opioid crisis. Some prescribers lowered opioid prescriptions and instead increased benzo use for anxiety, insomnia, or muscle spasms. This led to higher risks of co-prescribing benzos and opioids, which can increase the chance of overdose.
State data also shows that co-use of benzos with other substances is common in California. The most frequent combinations include benzos with opioids, alcohol, cannabis, and stimulants like methamphetamine. In 2022, over 70% of benzo-involved overdose deaths in California also involved opioids. When multiple substances are involved, comprehensive drug and alcohol treatment programs may be critical to address polysubstance dependencies effectively.
Demographic trends show that benzo misuse affects different groups in different ways. White non-Hispanic women over age 45 have higher rates of long-term prescription use, while young men in their twenties are more likely to misuse benzos recreationally. LGBTQ+ individuals and people experiencing homelessness are also identified as high-risk populations.
Benzodiazepines are classified as Schedule IV controlled substances in the United States. This means they have a recognized medical use but also carry a risk of dependence and addiction. Compared to substances like alcohol or opioids, benzos have a lower risk of overdose death when used alone, but can be highly addictive, especially when used long-term or without medical supervision.
In California, benzodiazepine prescriptions remain high. According to the California Department of Public Health, over 5 million benzodiazepine prescriptions were filled in 2022. Data from the Substance Abuse and Mental Health Services Administration (SAMHSA) show that around 2% of California residents reported misuse of tranquilizers, including benzos, in the past year.
Some risk factors that can increase a person’s vulnerability to benzo addiction include a history of substance use, co-occurring mental health conditions such as anxiety or depression, and prolonged or high-dose prescriptions. People who use benzos without a prescription or mix them with alcohol or opioids are also at higher risk.
Benzodiazepine tolerance can develop quickly, sometimes within just a few weeks of regular use. Tolerance means the body becomes less responsive to the drug, leading to reduced effects over time.
As tolerance increases, people may take higher doses to feel the same calming or sedative effects. This escalates the risk of both physical dependence and addiction.
Research published in the Journal of Clinical Psychiatry found that tolerance to the sleep-inducing effects of benzos can develop within 7 to 14 days. For some individuals, tolerance to the anti-anxiety effects may take slightly longer, but still often occurs within a few weeks.
Benzo withdrawal can be medically serious. When someone stops taking the drug after regular use, their body may react strongly, especially if the dose was high or used over a long period.
Medical supervision is often required during benzo withdrawal to reduce the risks of seizures, extreme anxiety, or other complications. Sudden discontinuation can be dangerous, especially with short-acting benzos like Xanax.
Withdrawal symptoms may vary by person, but common symptoms include anxiety, insomnia, irritability, muscle pain, tremors, and, in severe cases, seizures.

Benzodiazepine Addiction Treatment
Stopping benzodiazepines suddenly can cause serious symptoms, including seizures or death. Due to the risks, medical detox is completed under professional supervision.
Doctors use a tapering method to slowly reduce the dose over time. This helps lower the risk of severe withdrawal symptoms. The exact tapering schedule depends on the drug used, dosage, and how long the person has been taking it.
Medical staff monitor vital signs and manage symptoms such as anxiety, insomnia, or muscle pain. They may use other medications to support the taper process. The detox process can last from several days to a few weeks, depending on individual needs.
During residential treatment, individuals live at the facility while participating in daily therapy and support. This setting offers 24-hour care in a structured environment.
Inpatient rehab includes individual therapy, group therapy, medication management, and wellness-based services. During early recovery, constant support can help manage cravings and emotional distress.
Programs typically last 30 to 90 days. The length depends on how severe the addiction is and how the person responds to treatment.
Behavioral therapies help address how thoughts and emotions affect behaviors. These therapies are used during and after detox.
Cognitive behavioral therapy (CBT) helps identify and change unhelpful thinking patterns. Dialectical behavior therapy (DBT) focuses on emotional regulation and coping skills. Motivational Interviewing helps people explore their reasons for change. Group therapy offers peer support and shared experiences.
These types of addiction counseling focus on targeting the psychological factors that contribute to benzodiazepine addiction. They also teach new ways to manage stress, anxiety, and triggers.
Aftercare provides support after inpatient treatment ends. This phase helps people build long-term recovery skills.
Aftercare plans may include weekly therapy, alumni groups, or coaching sessions. Support groups like 12-step programs or SMART Recovery are often recommended. Family involvement may continue through therapy sessions or workshops.
Relapse prevention strategies are developed with each person. They include identifying triggers, building routines, and having a plan for setbacks. Continued care supports stability after benzo addiction treatment.
Polysubstance Use and Co-Occurring Disorders
Mixing benzodiazepines with alcohol or opioids increases the risk of overdose. These substances all slow down breathing and heart rate. When taken together, they can cause respiratory failure, coma, or death.
People with benzo addiction often have co-occurring mental health conditions. Anxiety disorders are common because benzodiazepines are often prescribed to manage anxiety. Over time, people may begin to rely on the drug instead of addressing the root causes of anxiety. Individuals facing both addiction and mental health concerns may benefit from dual diagnosis residential treatment to fully address underlying issues.
Depression is also frequently seen with benzo use. Long-term use of benzodiazepines can affect mood and sleep, which may worsen depressive symptoms. Some individuals may misuse benzos to escape emotional pain.
PTSD and insomnia are other conditions linked to benzo abuse. Benzodiazepines are sometimes used to manage trauma-related sleep problems or intrusive thoughts. This can lead to dependence if the underlying trauma is not addressed in therapy.
Integrated treatment uses a dual diagnosis approach. This means treating benzo addiction and mental health disorders at the same time. The approach includes medical care, psychiatric support, and evidence-based therapies. Treatment plans are individualized and adjusted over time.
Preventing Dependence on Benzodiazepines
Responsible prescribing practices help lower the risk of benzo addiction. Healthcare providers often prescribe the lowest effective dose for the shortest amount of time. When patients and prescribers work together, the risk of developing physical or psychological dependence can be reduced.
There are several strategies patients can follow when taking benzodiazepines:
- Take the exact dose prescribed by the provider. Do not take more or less than instructed.
- Attend regular follow-up appointments to review how the medication is working and whether adjustments are needed.
- Use benzodiazepines for a limited time whenever possible. Long-term use can increase dependence risk.
- Share any concerns about side effects or cravings with the healthcare provider. Honest communication supports safe use.
There are non-benzodiazepine options for treating anxiety and sleep problems. Some medications are non-addictive and may be suitable alternatives.
Therapy approaches, such as cognitive behavioral therapy for insomnia (CBT-I), help individuals change thought patterns and behaviors without medication. CBT is also used to treat anxiety disorders.
Lifestyle changes like regular exercise, consistent sleep routines, and limiting caffeine can improve sleep and mood. Stress management techniques, including mindfulness and structured breathing, may also help reduce anxiety.
At Peak Path Health, holistic care plans may include acupuncture, nutritional support, yoga, and trauma-informed therapy. These services can support individuals who are managing anxiety or recovering from benzo addiction.

Moving Forward with Evidence-Based Care
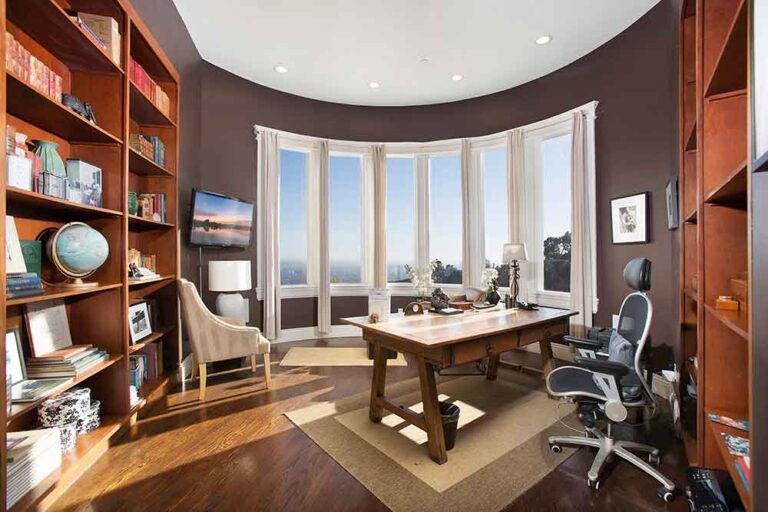
At Peak Path Health in Los Angeles, California, benzo addiction treatment combines medical detox, psychiatric care, individual therapy, and integrative wellness services. Care is delivered in our luxury addiction and mental health center in the Hollywood Hills, where privacy and comfort support the healing process. Each phase of treatment is guided by licensed clinical staff and tailored to the client’s current stability and long-term goals.
Treatment plans are developed individually. Clients participate in clinical assessments, psychiatric evaluations, and collaborative goal setting. This approach allows clinicians to respond to co-occurring conditions such as anxiety or trauma, which are often linked to benzo misuse.

Benzo Addiction and Treatment FAQs
Benzodiazepine withdrawal varies by individual, but acute symptoms typically last 2-4 weeks, while protracted withdrawal may continue for several months. Medical monitoring during withdrawal helps manage physical and psychological symptoms and reduces the risk of complications such as seizures or severe anxiety.
Peak Path Health uses a personalized, medically supervised model of care with treatment plans created based on each client’s physical, emotional, and psychological needs. Care is provided in a private setting in the Hollywood Hills, integrating evidence-based therapies with wellness practices to support long-term stability and address co-occurring mental health conditions.
Yes, physical dependence on benzodiazepines can happen even when the medication is taken according to a doctor’s instructions, particularly with long-term use (beyond 2-4 weeks). Regular follow-up with a healthcare provider helps detect signs of dependence early and allows for adjustments to be made accordingly.