Prescription drug addiction often begins innocently; a doctor prescribes medication for a person’s back pain or anxiety, but over time, the body and brain start needing more just to feel normal. For many individuals, what begins as a doctor’s prescription for pain management, anxiety relief, or focus improvement gradually transforms into a pattern of misuse that disrupts daily life. What makes prescription drug dependency so tricky to spot? These are not street drugs; they come with a doctor’s signature and a pharmacy label, creating a false sense of safety that can mask growing dependence.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), approximately 16 million Americans aged 12 and older misuse prescription drugs, with about 2 million classified as addicted. The three primary categories of commonly misused prescription medications include opioid painkillers, benzodiazepines for anxiety, and stimulants for attention disorders. While these medications affect different brain systems, they share one critical trait: they can all hijack the brain’s reward pathways and lead to physical dependence if not carefully monitored.
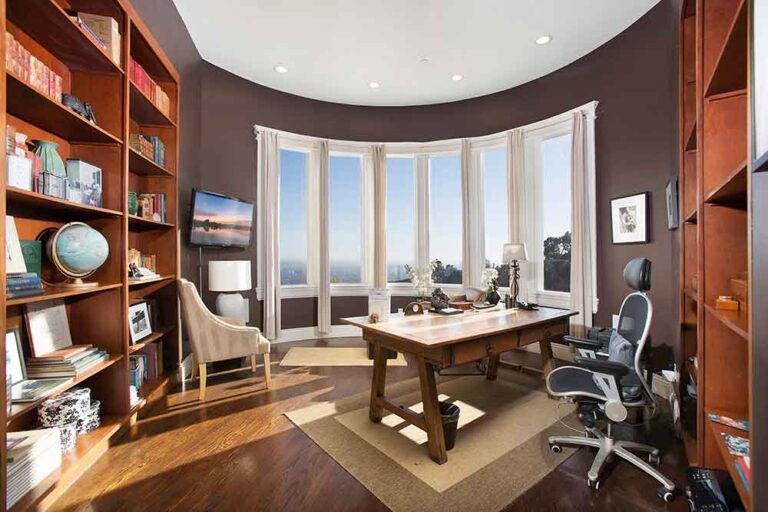
Peak Path Health’s prescription drug addiction treatment center, located in the Hollywood Hills and Woodland Hills of Los Angeles, California, addresses the complex nature of prescription medication dependence. Through comprehensive treatment services that combine medical supervision, psychiatric care, and evidence-based therapies, the center provides individualized support for professionals and individuals seeking recovery in a private, luxury setting.


Types of Prescription Drugs
Opioid painkillers are medications prescribed to manage moderate to severe pain following surgery, injury, or chronic conditions. These drugs bind to opioid receptors in the brain and spinal cord, blocking pain signals while creating feelings of euphoria or relaxation. Common opioid medications include oxycodone, hydrocodone, morphine, codeine, and fentanyl.
People can develop physical dependence in just two to three weeks of regular opioid use, even when following their prescription exactly. What’s happening? Their brains are essentially outsourcing pain control to the medication and shutting down natural endorphin production.
Benzodiazepines are medications prescribed for anxiety disorders, panic attacks, insomnia, and seizure disorders. These drugs work by enhancing the activity of gamma-aminobutyric acid (GABA), a neurotransmitter that slows brain activity and produces calming effects. Common benzodiazepines include alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), and clonazepam (Klonopin). Benzodiazepines can create physical dependence within two to four weeks of regular use, even at prescribed doses.
Prescription stimulants are medications used to treat attention-deficit/hyperactivity disorder (ADHD) and narcolepsy. These drugs increase dopamine and norepinephrine levels in the brain, improving focus, attention, and wakefulness. Common stimulant medications include amphetamine/dextroamphetamine (Adderall), methylphenidate (Ritalin), and lisdexamfetamine (Vyvanse). Misuse often involves taking higher doses than prescribed, using someone else’s prescription, or crushing and snorting pills to intensify effects.
Signs and Symptoms of Prescription Drug Abuse
Clinicians assessing for prescription dependence look for telltale physical signs, which vary by drug type but follow recognizable patterns:
- Tolerance: The body becomes less responsive to the medication over time, leading to increased dosage needs.
- Withdrawal symptoms: Physical reactions such as nausea, sweating, tremors, or insomnia occur when medication is reduced or stopped.
- Physical health changes: Alterations in sleep quality, eating habits, or noticeable weight fluctuations appear without other explanation.
Behavioral shifts often accompany prescription drug abuse as obtaining and using medication becomes a priority:
- Doctor shopping: Seeking prescriptions from multiple providers to maintain access to medications
- Increased secrecy: Concealing medication use, lying about dosages, or becoming defensive about prescription habits
- Neglecting responsibilities: Missing work deadlines, avoiding family commitments, or falling behind on obligations
Psychological dependence on prescription medications creates patterns where thoughts and emotions center around the next dose:
- Preoccupation with medication: Persistent thoughts about the next dose or when to take medication
- Anxiety when supply is low: Fear, panic, or distress about running out of prescriptions
- Mood swings: Irritability, depression, or sudden emotional changes that seem unrelated to external circumstances


Causes and Risk Factors
Certain prescribing practices can increase the likelihood of developing dependence on prescription medications. Extended prescription durations expose individuals to prolonged medication use, which allows physical dependence to develop gradually. Higher prescribed doses create stronger effects in the body and brain, making tolerance and dependence more likely to occur. Multiple overlapping prescriptions can compound addiction risk, particularly when different medications affect similar brain systems.
Mental health disorders significantly increase vulnerability to prescription drug addiction. Individuals with anxiety disorders may use prescription medications to manage symptoms, creating a pattern of psychological dependence. According to the National Institute of Mental Health (NIMH), generalized anxiety disorder symptoms affect 7.4% of adults, highlighting the prevalence of conditions that may lead to prescription medication use and potential misuse.
Genetic factors play a significant role in addiction vulnerability, with family history indicating an inherited predisposition to substance use disorders. Early life trauma and chronic stress increase susceptibility to developing dependence on prescription medications. Environmental influences such as peer pressure and early exposure to drugs create additional risk pathways.
Effects of Prescription Drug Addiction
Short-term effects of prescription drug addiction can appear quickly and vary based on the type of medication involved:
- Respiratory depression: Opioids and benzodiazepines commonly cause slowed breathing, which reduces oxygen levels in the body
- Cognitive impairment: Difficulty concentrating, memory problems, or confusion that interferes with work and daily decision-making
- Accidents and injuries: Impaired judgment, slowed reaction times, and coordination problems increase the risk of falls and vehicle accidents
According to the California Department of Public Health, in 2023, there were 53,555 emergency department visits related to non-fatal drug overdoses, many involving prescription medications.
Long-term prescription drug use can cause lasting damage to major organs. Opioids and other prescription medications may lead to liver complications, kidney dysfunction, and cardiovascular problems. These conditions often develop gradually and may not be immediately noticeable until significant damage has occurred.
Brain changes represent another serious long-term consequence of prescription drug addiction. Chronic use alters brain chemistry and function, particularly in areas related to reward, motivation, and decision-making.
Career consequences often emerge as prescription drug addiction progresses. Absenteeism increases as individuals miss work due to drug use, withdrawal symptoms, or related health problems. Decreased performance becomes noticeable when cognitive impairment and physical symptoms interfere with job responsibilities.
Family strain develops as prescription drug addiction affects trust and communication. Conflict arises when family members discover hidden medication use or notice personality changes. Treatment access remains limited in Los Angeles, with only about 0.8% of adults with substance use disorder receiving care, leaving over 94% untreated.


Comprehensive Treatment at Peak Path Health
Attempting to detox from prescription medications without professional help is not advised. Quitting certain medications abruptly without medical supervision can lead to dangerous, sometimes fatal, complications. Stopping certain medications abruptly, particularly opioids and benzodiazepines, can cause severe physical reactions, including seizures, respiratory distress, or cardiovascular complications.
Medical detox provides the safest environment for individuals to begin recovery from prescription drug addiction. Professional detox programs reduce risks by providing 24-hour monitoring and evidence-based withdrawal management protocols. The detox process typically lasts 5 to 10 days, though timelines vary based on the specific medication, dosage history, and individual health factors.
Prescription drug addiction treatment relies on structured therapeutic approaches that address both the psychological patterns driving substance use and the skills needed for long-term recovery. Behavioral therapies help individuals understand the connection between thoughts, emotions, and substance use behaviors.
Cognitive Behavioral Therapy (CBT) focuses on identifying and changing thought patterns that contribute to prescription drug misuse. The therapy helps clients recognize situations, emotions, or beliefs that trigger cravings or lead to relapse. Through structured sessions, individuals learn to challenge distorted thinking and replace unhealthy patterns with more adaptive responses.
Dialectical Behavior Therapy (DBT) combines cognitive-behavioral techniques with mindfulness practices to address emotional dysregulation. Originally developed for individuals with intense emotional experiences, DBT has proven effective in treating substance use disorders, including prescription drug addiction.
Prescription drug addiction treatment extends beyond medical detox and behavioral therapy. Holistic approaches address the physical, emotional, and psychological effects of long-term prescription drug misuse. Integrated wellness practices complement evidence-based care to support comprehensive recovery.
Mindfulness techniques teach individuals to observe thoughts and physical sensations without judgment. For people recovering from prescription drug addiction, these practices help manage cravings and reduce the anxiety that often triggers relapse. Nutritional therapy restores physical health through balanced meals designed to support healing and stabilize mood.
Dual Diagnosis and Co-Occurring Disorders
Anxiety and depression frequently co-occur with prescription drug addiction. People may initially receive prescriptions for benzodiazepines or opioids to manage anxiety symptoms or chronic pain linked to depression. Over time, physical dependence can develop, even when medications are taken as prescribed.
Integrated care combines psychiatric support, medication management, and evidence-based therapies to address both addiction and mental health symptoms. Addressing underlying anxiety or depression reduces the likelihood of returning to prescription drug use after treatment ends.


Aftercare and Relapse Prevention
Transition support includes coordinating outpatient therapy, medication management appointments, and psychiatric follow-up care. Clients receive referrals to community-based services such as sober living facilities, vocational programs, and peer support groups.
Alumni programs provide ongoing connection and accountability after residential treatment ends. Graduates of the program can participate in monthly alumni meetings, virtual check-ins, and recovery-focused social events. Staying engaged with a recovery community helps individuals maintain motivation and access support during difficult periods.
Why Choose Prescription Drug Addiction Treatment in Los Angeles
The clinical team at Peak Path Health includes board-certified psychiatrists, licensed therapists, and medical professionals experienced in treating prescription drug addiction and co-occurring disorders. Neuropsychological testing helps identify cognitive patterns, attention deficits, or trauma-related symptoms that may contribute to medication misuse.
Confidentiality protocols at Peak Path Health protect client privacy throughout treatment. The center serves professionals, executives, and individuals whose careers or public profiles require discretion during recovery. All staff members adhere to strict privacy standards, and treatment occurs in private settings away from public view.
Recovery is Possible at Peak Path Health
If you or a loved one is dealing with prescription drug addiction, support is available. Reach out to our team to learn more about taking the next step toward recovery.